Rétinopathie diabétique
Les complications ophtalmologiques du diabète sont une cause majeure de malvoyance et de cécité.
La rétinopathie diabétique
en France
50 % des diabétiques de type 2
1,5 million
de patients
Physiopathologie
Le diabète est une maladie qui provoque une hyperglycémie chronique (hausse anormale du taux de sucre dans le sang). Cette hyperglycémie, entraine une inflammation chronique des capillaires rétiniens qui aboutit à leur occlusion.
L’occlusion du capillaire entraine ce qu’on appelle une ischémie rétinienne, c'est-à-dire a une insuffisance d’apport sanguin au niveau de la rétine.
L’ischémie rétinienne quand elle est importante, est le point d’appel d’une néovascularisation, c'est-à-dire, la formation de vaisseaux anormaux au sein de la rétine. Ces néovaisseaux sont redoutables, car ils se compliquent d’hémorragie, de décollement de rétine voire de glaucome néovasculaire. Ces complications sont dramatiques puisqu’elles peuvent entrainer une cécité.
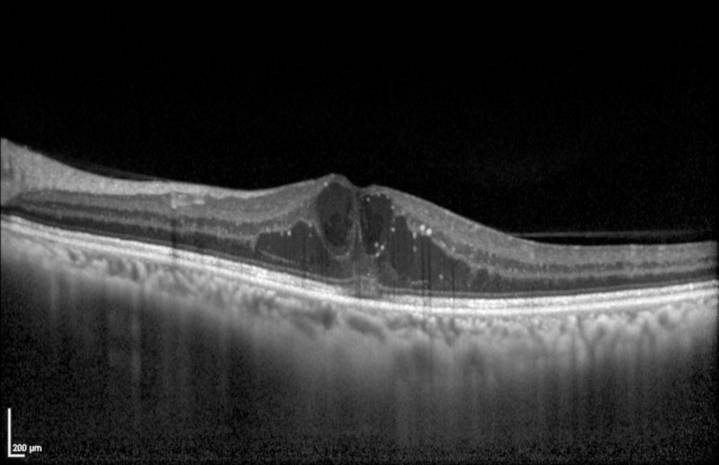
Le diabète peut aussi provoquer des altérations au niveau de la macula. La macula est le centre de la rétine, c’est la zone de la rétine qui permet de voir une image nette. Au niveau maculaire, le diabète peut entrainer une accumulation anormale de fluide, ce qu’on appelle œdème maculaire qui entraine une baisse de vision.
Diagnostic
Longtemps, la rétinopathie diabétique est asymptomatique. C’est pour cela qu’il est indispensable que tous les patients diabétiques fassent contrôler leur fond d’œil.
Le diagnostic de rétinopathie diabétique se fait en général sur le fond d’œil. D’autres examens peuvent être nécessaires pour évaluer la sévérité de la rétinopathie diabétique comme l’OCT (tomographie en cohérence optique), l’angiographie voire l’OCT angiographie.
L’OCT est aujourd’hui est indispensable pour diagnostiquer l’œdème maculaire diabétique.
Évolution de la maladie
On distingue plusieurs stades de rétinopathie diabétique :
- Rétinopathie diabétique non proliférante minime, modérée ou sévère, où on retrouve des microanévrysmes, des hémorragies, des veines dilatées.
- Rétinopathie diabétique proliférante, où on retrouve la présence de néovaisseaux sur la rétine.
- La rétinopathie diabétique proliférante peut se compliquer d’hémorragie intra vitréene, de décollement de rétine tractionnel voire de glaucome néovasculaire.


Traitements
La premier traitement est l’équilibre strict du diabète et de la tension artérielle afin d’éviter l’aggravation des lésions.
Le traitement laser par photocoagulation pan-rétinienne est un traitement préventif de la rétinopathie diabétique qui a pour but de détruire les zones ischémiques, afin d’éviter une néovascularisation. Plusieurs séances sont nécessaires et leur rythme est fonction de la sévérité.
Un traitement chirurgical (vitrectomie) est indiqué en cas complication tel que l’hémorragie intra-vitréenne ou de décollement de rétine.
Concernant l’œdème maculaire à l’origine de baisse de vision, les injections intravitréennes de corticoïdes ou d’anti-VEGF sont aujourd’hui le traitement de référence.
Vous pouvez prendre rendez-vous avec un des ophtalmologistes du service qui prend en charge cette pathologie :
















