Occlusions veineuses rétiniennes
Qu’est-ce qu’une occlusion veineuse rétinienne ?
C’est la conséquence d’un ralentissement soudain de la circulation sanguine dans les veines de la rétine, qui peut avoir un retentissement sur l’ensemble de la circulation sanguine de la rétine, en particulier, en amont, sur la circulation du sang dans les capillaires et dans les artérioles rétiniennes. La perturbation de l’oxygénation de la rétine est à l’origine de troubles visuels plus ou moins sévères.
L’occlusion de la veine centrale de la rétine a des conséquences plus graves qu’une occlusion d’une branche veineuse qui ne concerne qu’une partie plus petite de la rétine.
Parmi les causes les plus souvent rencontrées, on retrouve les facteurs de risques vasculaires comme l’hypertension artérielle, l’augmentation du taux de lipides (graisses) sanguins, le diabète, le tabagisme, le surpoids, mais aussi l’élévation de la tension oculaire (glaucome). L’apnée du sommeil est un facteur favorisant souvent rencontré.
Diagnostic et évolution
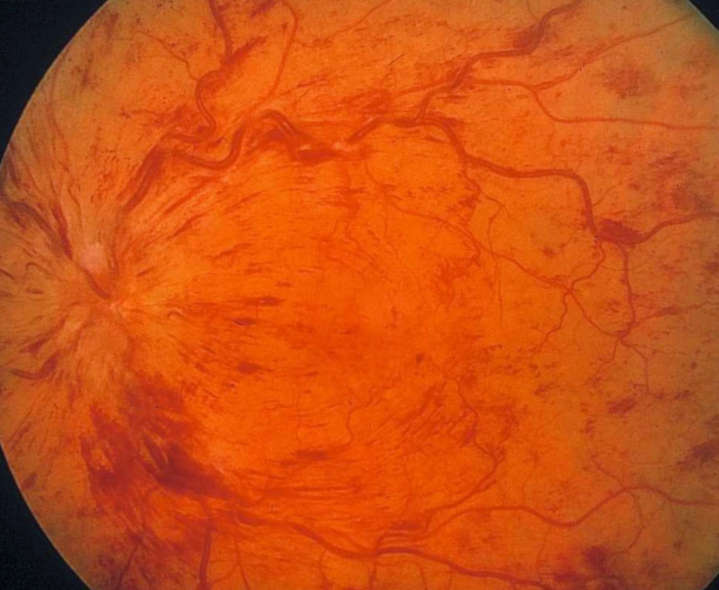
Si l’occlusion veineuse rétinienne est suspectée dès l’examen du fond d’œil, il est très utile de confirmer le diagnostic par une angiographie à la fluorescéine qui met parfaitement en évidence la circulation sanguine dans les vaisseaux rétiniens et en analyse les conséquences. La tomographie en cohérence optique (OCT) apporte des informations utiles pour évaluer l’œdème maculaire qui est une conséquence très fréquente des occlusions veineuses.
L’évolution des occlusions de la veine centrale de la rétine est très variable
Il y a une possibilité de récupération complète ou quasi complète dans environ 20 % des cas ou, à l’opposé, un risque de baisse majeure de la vision.
La durée d’évolution des occlusions de la veine centrale de la rétine peut se résumer à quelques semaines pour les cas les plus favorables, ou devenir chronique dans les cas d’aggravation lente et progressive.
Quel est le traitement initial des occlusions de la veine centrale de la rétine ?
Plusieurs traitements peuvent être proposés. Le traitement des facteurs de risque est fondamental pour éviter le risque de rechute ou d’atteinte de l’autre œil (10 à 15 % des cas environ).
Les traitements anti-œdémateux administrés par injection intra-vitréennes dans l’œil sont maintenant souvent prescrits pour traiter l’œdème maculaire et permettent d’améliorer la vision dans la majorité des cas ; les injections doivent être démarrées rapidement dans les cas sévères.
Le traitement au laser est indiqué dans certains cas, principalement pour éviter les complications des formes ischémiques ou pour le traitement des œdèmes récidivants dans les occlusions de branche veineuse.
Vous pouvez prendre rendez-vous avec un des ophtalmologistes du service qui prend en charge cette pathologie :

Dr Sorana PacurariuAssistant Spécialiste
















